Connect With Us

Symptoms and Risks of Toenail Fungus

Fungal toenail infections, although not typically serious, can be quite persistent and challenging to treat. These infections often begin at the edge of the toenail, gradually spreading and causing the nail to become brittle, thickened, and discolored. You may notice your nails turning yellow or white, becoming crumbly, and even lifting off the nail bed, which can be accompanied by swelling and pain. Risk factors include consistently warm and damp feet, wearing tight or non-breathable shoes, and sharing personal items like nail clippers or towels. Untreated fungal toenails can lead to more serious health issues, and for severe or resistant fungal toenail infections, minor surgical procedures to remove the affected nail might be necessary. If you suspect a fungal toenail infection, especially if you have underlying health conditions, it is suggested that you schedule an appointment with a podiatrist to begin a tailored treatment plan.
For more information about treatment, contact Robert Hutchison, DPM, FACFAS of Lower Keys Foot & Ankle Surgery. Our doctor can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact our office located in Key West, FL . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Toenail Fungus
Toenail fungus is a frustrating problem that affects many people. It can be persistent and hard to get rid of. As many different types of fungi are present throughout the environment, it is very easy to contract toenail fungus.
The feet are especially susceptible to toenail fungus because shoes and socks create the ideal dark and moist environment that fungal infections thrive in. While fungal infections of the nail plate are quite common, if left untreated they can spread beyond the toenail and into the skin and other parts of the body.
Signs of toenail fungus include a thickened nail that has become yellow or brown in color, a foul smell, and debris beneath the nail. The toe may become painful due to the pressure of a thicker nail or the buildup of debris.
Treatment for toenail fungus is most effective during the early stages of an infection. If there is an accumulation of debris beneath the nail plate, an ingrown nail or a more serious infection can occur. While each treatment varies between patients, your podiatrist may prescribe you oral medications, topical liquids and creams, or laser therapy. To determine the best treatment process for you, be sure to visit your podiatrist at the first signs of toenail fungus.
Causes and Symptoms of Athlete’s Foot

Athlete's foot, caused by the fungus Trichophyton, flourishes in warm and damp environments. This fungus, usually harmless on the skin, can rapidly multiply when feet are confined in tight, non-breathable shoes, particularly plastic ones, or when socks remain damp. It spreads through direct skin contact, as well as indirectly via contaminated surfaces, like showers, pools, towels, and bedding. Symptoms of athlete's foot infections typically include itching, stinging, and burning sensations between the toes, in addition to dry, flaky, red, and scaly skin. In advanced cases, the skin may crack, ooze, or develop blisters. Athlete’s foot, which is highly contagious, can spread to the soles and sides of the feet, or even to the hands. Anyone with a weakened immune system is at a greater risk. Prompt treatment is vital to prevent the infection from spreading and worsening. If left untreated, athlete’s foot can lead to bacterial infections derived from skin fissures. For persistent symptoms, it is suggested that you schedule an appointment with a podiatrist for an exam and tailored treatment plans to effectively manage and eradicate the infection.
Athlete’s foot is an inconvenient condition that can be easily reduced with the proper treatment. If you have any concerns about your feet and ankles, contact Robert Hutchison, DPM, FACFAS from Lower Keys Foot & Ankle Surgery. Our doctor will treat your foot and ankle needs.
Athlete’s Foot: The Sole Story
Athlete's foot, also known as tinea pedis, can be an extremely contagious foot infection. It is commonly contracted in public changing areas and bathrooms, dormitory style living quarters, around locker rooms and public swimming pools, or anywhere your feet often come into contact with other people.
Solutions to Combat Athlete’s Foot
- Hydrate your feet by using lotion
- Exfoliate
- Buff off nails
- Use of anti-fungal products
- Examine your feet and visit your doctor if any suspicious blisters or cuts develop
Athlete’s foot can cause many irritating symptoms such as dry and flaking skin, itching, and redness. Some more severe symptoms can include bleeding and cracked skin, intense itching and burning, and even pain when walking. In the worst cases, Athlete’s foot can cause blistering as well. Speak to your podiatrist for a better understanding of the different causes of Athlete’s foot, as well as help in determining which treatment options are best for you.
If you have any questions please feel free to contact our office located in Key West, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Athlete's Foot
Athlete’s foot is an extremely contagious infection caused by a fungus that results in itching, burning, dry, and flaking feet. The fungus that causes athlete’s foot is known as tinea pedis and thrives in moist, dark areas such as shower floors, gyms, socks and shoes, commons areas, public changing areas, bathrooms, dormitory style houses, locker rooms, and public swimming pools. Athlete’s foot is difficult to treat as well because of the highly contagious and recurrent nature of the fungus.
Tinea is the same fungus that causes ringworm, and is spread by direct contact with an infected body part, contaminated clothing, or by touching other objects and body parts that have been exposed to the fungus. Because the feet are an ideal place for tinea to grow and spread, this is the most commonly affected area. It is, however, known to grow in other places. The term athlete’s foot describes tinea that grows strictly on the feet.
The most commonly infected body parts are the hands, groin, and scalp, as well as the feet. Around 70% of the population suffer from tinea infections at some point in their lives, however not all of these cases are athlete’s foot. Just like any other ailment, some people are more likely to get it than others, such as people with a history of tinea infections or other skin infections, both recurring and non-recurring ones. The extent to which a person experiences regrowth and recurrent tinea infections varies from person to person.
Sometimes people will not even know that they are infected with tinea or that they have athlete’s foot because of a lack of symptoms. However, most experience mild to moderate flaking, itching, redness, and burning. However, some of the more severe symptoms include cracking and bleeding skin, intense itching and burning, pain while walking or standing, and even blistering.
Because of the recurring nature of the tinea fungus and the athlete’s foot it causes, the best way to treat this condition is with prevention. You can take some preventative measures such as wearing flip flops or sandals in locker rooms and public showers to reduce contact with the floor. It also helps to keep clean, dry feet while allowing them to breathe. Using powders to keep your feet dry is a good idea, as well as keeping your feet exposed to light and cool air, to prevent the growth of tinea. If you do happen to get athlete’s foot, opt for using topical medicated creams, ointments or sprays. These treatments help eliminate and prevent it from coming back.
How Podiatrists Help With Diabetic Foot Care
 Podiatrists play a key role when it comes to managing and preventing foot-related complications in diabetes patients. Foot issues are a common occurrence in diabetics, due to the poor blood circulation and nerve damage, or neuropathy, that often accompany the disease. Podiatrists specialize in early detection and treatment of potential foot problems like ulcers, infections, and structural issues. This makes regular check-ups with podiatrists important for someone who is at risk for these issues. During visits, a podiatrist will conduct comprehensive foot exams to look for signs of decreased circulation, changes in foot structure, or nerve damage. This foot doctor can provide guidance on proper foot care practices, such as how to safely trim nails and avoid injuries. Podiatrists may also recommend appropriate footwear to prevent pressure sores and injuries. Additionally, podiatrists can treat any current foot problems to prevent them from escalating into more serious conditions that could lead to amputation. By closely monitoring the health of a diabetic's feet, podiatrists help maintain mobility and prevent life-threatening complications. If you are at risk for foot complications due to diabetes, it is suggested that you add a podiatrist to your regular care team.
Podiatrists play a key role when it comes to managing and preventing foot-related complications in diabetes patients. Foot issues are a common occurrence in diabetics, due to the poor blood circulation and nerve damage, or neuropathy, that often accompany the disease. Podiatrists specialize in early detection and treatment of potential foot problems like ulcers, infections, and structural issues. This makes regular check-ups with podiatrists important for someone who is at risk for these issues. During visits, a podiatrist will conduct comprehensive foot exams to look for signs of decreased circulation, changes in foot structure, or nerve damage. This foot doctor can provide guidance on proper foot care practices, such as how to safely trim nails and avoid injuries. Podiatrists may also recommend appropriate footwear to prevent pressure sores and injuries. Additionally, podiatrists can treat any current foot problems to prevent them from escalating into more serious conditions that could lead to amputation. By closely monitoring the health of a diabetic's feet, podiatrists help maintain mobility and prevent life-threatening complications. If you are at risk for foot complications due to diabetes, it is suggested that you add a podiatrist to your regular care team.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact Robert Hutchison, DPM, FACFAS from Lower Keys Foot & Ankle Surgery. Our doctor can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our office located in Key West, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
How to Care for Diabetic Foot
Millions of people are affected by diabetes each year. Diabetes damages blood vessels in all parts of the body, especially the feet. The legs and feet may develop slow blood flow, which causes neuropathy, or nerve damage. Once a diabetic patient develops neuropathy, it is important that the feet are well taken care of. Otherwise, the lower limbs may have to be amputated. This only happens in drastic cases, but it shows how seriously diabetic foot care should be taken.
It is very important to always wash and dry the feet thoroughly, especially in between the toes, if you’re a diabetic. Secondly, examining your feet and toes for redness or sores must be done, even if you do not feel pain. You may also want to examine your feet from the bottom. Try to avoid wearing colored socks to prevent infections that may occur from the dye. Well-fitting socks are also highly recommended.
A diabetic’s physician should always monitor their blood levels to test how well blood sugars are being maintained. In addition to giving advice about everyday eating habits and foot care, a physician may prescribe medicine to help with the diabetic patient’s neuropathy. It is also advised to see a podiatrist if experiencing any feet conditions. Toenails may also need to be taken care of by a podiatrist. This prevents patients from cutting too deeply around their cuticles, which can lead to infection.
A person can take care of their feet at home by following the instructions of their physician. Using creams on one’s feet is also an effective way to heal dryness. Proceed with caution when using tools to remove calluses, as severe diabetics may not be able to feel pain on their feet. If any complications arise do not hesitate to contact a podiatrist.
On a daily basis, diabetic feet must be checked. If you are ever concerned about something, contact your health care professional. You never want to wait until a wound becomes too severe to treat. If left untreated, gangrene may develop. Gangrene is a serious infection that can lead to sepsis or amputation. It is also important for diabetics to be on the lookout for ulcers. Ulcers are sores that develop from tissue loss on the skin. They can be quite painful and require intensive treatment. Early treatment and everyday inspection are imperative to staying healthy.
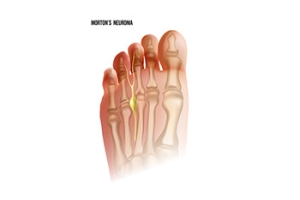
Facts About Morton's Neuroma
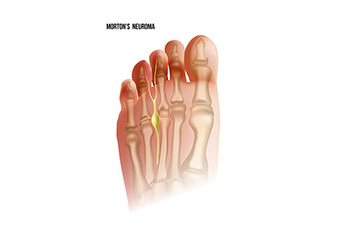
Morton's neuroma, a condition often misunderstood, affects the foot's nerves, particularly between the third and fourth toes. This ailment, named after Thomas George Morton, a 19th-century American surgeon, causes discomfort and pain. The pain is often likened to walking on a pebble or having a fold in the sock. The sensation arises due to the thickening of the tissue surrounding the nerves, leading to irritation and inflammation. Although high-heeled shoes and tight footwear worsen symptoms, anyone can develop Morton's Neuroma. Interestingly, it is not a true neuroma, but rather a perineural fibrosis, which is a thickening of nerve tissue. Diagnosis typically involves clinical evaluation and imaging studies, with treatment options ranging from orthotics and shoe modifications to more invasive procedures like injections or surgery in more severe cases. If you have pain in this part of your foot, it is suggested that you consult a podiatrist who can diagnose and offer correct treatment solutions for Morton’s neuroma.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Robert Hutchison, DPM, FACFAS of Lower Keys Foot & Ankle Surgery. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Key West, FL . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
Morton's Neuroma, also called Intermetatarsal Neuroma or Plantar Neuroma, is a condition that affects the nerves of the feet, usually the area between the third and fourth toe. Neuroma refers to a benign growth that can occur in different parts of the body. Morton's Neuroma strictly affects the feet. This condition causes the tissue around the nerves that lead to the toes becoming thick, causing pain in the ball of the foot.
This condition can be caused by injury, pressure or irritation. Normally no lump will be felt, but instead burning pain in the ball of the foot will be experienced. Numbness and tingling may also occur. With the onset of this condition, a person may feel pain when tight or narrow shoes are worn. As the condition worsens, the pain may persist for days, or even weeks.
Persistent foot pain should always be a concern. The foot should be examined by a podiatrist if pain persists longer than a few days with no relief from changing shoes. The earlier the foot is examined and treated, the less chance there will be for surgical treatment.
There are some factors that can play a role in the development of Morton's Neuroma. These include wearing ill-fitting shoes that cause pressure to the toes, such as high heels. Also, high impact exercise may contribute to the cause of this condition. Morton’s Neuroma may also develop if the foot sustains an injury. Another cause includes walking abnormally due to bunions or flat feet. This causes excessive pressure and irritates the tissue. At times, people are affected for no determinable reason.
Podiatrists can alleviate the effects of this condition using a treatment plan to help decrease the pain and heal the foot tissue. Depending upon the severity of the Morton's Neuroma, the treatment plan can vary. For cases that are mild to moderate, treatments may include applying padding to the arch to relieve pressure from the nerve and reduce compression while walking. Ice packs can also help reduce swelling. The podiatrist may also create a custom orthotic device to support the foot and reduce compression and pressure on the affected nerve. The doctor will probably advise against partaking in activities that cause constant pressure on the affected area. They may provide wider shoes to ease the pressure from the toes. If these treatments do not relieve the symptoms of this condition, the doctor may use injection therapy.
Surgical treatment may be recommended by the podiatrist if all other treatments fail to provide relief. Normally, the podiatric surgeon will decide on either a surgical procedure that involves removal of the affected nerve or will choose surgery to release the nerve. After examination, the surgeon will decide on the best approach to treat the problem.
Recovery varies according to the type of surgical procedure. The patient will also be instructed on the best shoe wear to prevent the return of this condition, along with changes to workout routines, if this was a cause. Preventative measures are important in ensuring the condition does not return.
Fascinating Facts About Feet

Feet are remarkable structures comprising 26 bones, 33 joints, and more than 100 muscles, tendons, and ligaments. These bones are divided into three groups, consisting of the tarsal bones, which form the back of the foot and ankle, the metatarsal bones, which make up the midfoot, and the phalanges, which form the toes. On average, a person takes approximately 8,000 to 10,000 steps per day, which adds up to about 115,000 miles in a lifetime. Among the many joints in the feet, some of the most essential include the ankle joint, subtalar joint, and metatarsophalangeal joints. These joints work together to provide support, flexibility, and propulsion during movement, allowing us to walk, run, jump, and dance with ease. If you have developed foot pain which may be due to your foot's structure, it is suggested that you confer with a podiatrist who can help you with relief solutions.
If you have any concerns about your feet, contact Robert Hutchison, DPM, FACFAS from Lower Keys Foot & Ankle Surgery. Our doctor can provide the care you need to keep you pain-free and on your feet.
Biomechanics in Podiatry
Podiatric biomechanics is a particular sector of specialty podiatry with licensed practitioners who are trained to diagnose and treat conditions affecting the foot, ankle and lower leg. Biomechanics deals with the forces that act against the body, causing an interference with the biological structures. It focuses on the movement of the ankle, the foot and the forces that interact with them.
A History of Biomechanics
- Biomechanics dates back to the BC era in Egypt where evidence of professional foot care has been recorded.
- In 1974, biomechanics gained a higher profile from the studies of Merton Root, who claimed that by changing or controlling the forces between the ankle and the foot, corrections or conditions could be implemented to gain strength and coordination in the area.
Modern technological improvements are based on past theories and therapeutic processes that provide a better understanding of podiatric concepts for biomechanics. Computers can provide accurate information about the forces and patterns of the feet and lower legs.
Understanding biomechanics of the feet can help improve and eliminate pain, stopping further stress to the foot.
If you have any questions please feel free to contact our office located in Key West, FL . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.